by Dr. M | Mar 12, 2020 | Appointment, Exam, Glaucoma, Mark Moran, Medical Eye Care
As part of your comprehensive eye exam, we check the pressure of your eye, the Intraocular Pressure (IOP). This test, called tonometry, is one way to see if you are at risk for glaucoma. Regular screenings are a simple way to monitor your eye health. Early detection is essential in the treatment of glaucoma, since many times there are no symptoms with increased pressure, unless it is sudden.
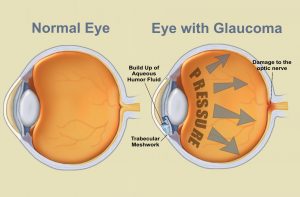
UNDERSTANDING EYE PRESSURE:
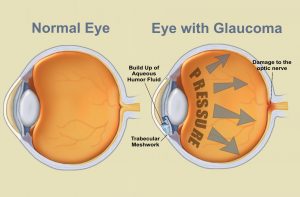
Inside the eye, there is a cycle of fluid production and fluid drainage. This fluid, in the front part of your eye, is called the aqueous humor. The aqueous humor nourishes your eye and helps it to keep its shape. If this cycle is out of balance, and more fluid is produced than can drain effectively, IOP increases. Over time, this increased eye pressure may cause damage to the optic nerve. A general guideline for normal eye pressure is between 10 and 21 mm/hg.
HOW WE MEASURE EYE PRESSURE:
 In our office, we measure eye pressure by instilling a drop that numbs your eye. Using a blue light, we then use an applanation tonometer that gently touches the surface of your eye. This painless test is a very effective way of measuring your pressure. It is helpful for the patient to relax and breathe normally while we perform this test.sisipisi.ccsisipisi.ccsisipisi.ccsisipisi.ccsisipisi.cc.
In our office, we measure eye pressure by instilling a drop that numbs your eye. Using a blue light, we then use an applanation tonometer that gently touches the surface of your eye. This painless test is a very effective way of measuring your pressure. It is helpful for the patient to relax and breathe normally while we perform this test.sisipisi.ccsisipisi.ccsisipisi.ccsisipisi.ccsisipisi.cc.
Although there are many other ways of measuring eye pressure, many people are familiar with the “puff of air test”. This test, called non-contact tonometry, uses a rapid air pulse to flatten the cornea. Your pressure is measured by detecting the force of the air against your eye. Although we don’t use this process, often when we ask patients them to “put your chin in the chin rest and forehead against the band” they worry we are going to puff air at them. They don’t seem to like it!
We can’t emphasize enough the importance of comprehensive eye exams. It is especially important to have an eye exam if you have a family history of eye disease, diabetes or high blood pressure. The best way to protect your vision is to come in for an exam, where Dr. Moran will evaluate your risk for disease and advise you of the optimal schedule of visits to protect your eye health.
Schedule your exam today, by calling our office at 610-628-2022, or by filling out the form on the website.
by Dr. M | Feb 4, 2020 | Cornea, Dry Eye, Exam, Medical Eye Care, Sun Damage, Surgery, Vision
There is an eye condition called “Surfer’s Eye”. Can you guess how it got its name?

It’s not about the water…but If you thought it had to do with too much sun exposure, you would be right!
Long-term exposure to UV rays from the sun, as well as wind and dust, may result in growths on the surface of the eye. Surfers are particularly vulnerable, since they spend their time in the sun without sunglasses or other eye protection.
The technical term for growths on the eye caused by sun exposure are called Pinguecula and Pterygium. The condition appears on the eye’s conjuctiva (the clear covering over the white part of the eye.
 Pinguecula is a yellowish, raised growth on the conjunctiva. It’s usually on the side of the eye near your nose, but can happen on the other side too. A pinguecula is an abnormality formed by protein deposits, calcium or fat. It’s like a callus on your finger or toesisipisi.ccsisipisi.ccsisipisi.ccsisipisi.cc.
Pinguecula is a yellowish, raised growth on the conjunctiva. It’s usually on the side of the eye near your nose, but can happen on the other side too. A pinguecula is an abnormality formed by protein deposits, calcium or fat. It’s like a callus on your finger or toesisipisi.ccsisipisi.ccsisipisi.ccsisipisi.cc.

Pterygium (Surfer’s Eye) is a growth of fleshy tissue (has blood vessels). It usually has a triangular shape. It can remain small or grow large enough to cover part of the cornea. When it grows into the cornea, it can interfere with your vision.
Symptoms
The symptoms of pinguecula and pterygium can range from mild to severe. They include:
- redness and swelling of the conjunctiva
- a yellow spot or bump that builds on the white of your eye
- dryness, itching and burning in the eye.
- sensation of something in the eye
Treatment
- The best treatment is prevention…keep your eyes lubricated with artificial tears and wear sunglasses with UV protection.
- If you have the condition, lubricating eye drops will help to reduce discomfort.
- Your doctor can prescribe steroid eye drops which may reduce inflammation, redness and swelling in the eye.
- Surgical Removal: If eye drops alone don’t alleviate the symptoms, or if the growth is large enough to interfere with your vision, the growth can be removed surgically.
Protect your eyes, protect your vision. If you have any questions about caring for your sight, email, call or text our office. We are here to help!
by Dr. M | Aug 6, 2019 | Cost, Education, Medical Eye Care, Medication, Patient Care, Prescriptions, Uncategorized

Talk to your pharmacist…you’ll be glad you did!
Have you spoken to your pharmacist lately? We know that prescription medications can be expensive. Your pharmacist can help you manage your medications, and may be able to help you find savings on your prescriptions.
Make friends with your pharmacist.
Your pharmacist is an essential part of your healthcare team. They may be aware of resources that can save you money, all you have to do is ask! Ask if you can speak with your pharmacist, they are happy to take a few minutes to review your medications. Most pharmacies have a private place for patient consultations.
Discount PROGRAMS.
Your pharmacist might be aware of discount programs that can save you money. They have a complete list of your medications, so they can can review the list with you. Talk to the pharmacy staff to see if there are any discount plans or strategies that might help you save some money.
ASK YOUR DOCTOR.
Ask your doctor if you there is a generic version of the medication. Generics are less expensive, and have the same active ingredients as the brand-name medications.
We want you to stay on track with the medications that are prescribed for you. The first step toward that goal is making sure that you get the medications that you need to stay healthy.
We know that an informed patient makes the best healthcare decisions, so make sure ask questions! You can benefit from relationships with every member of your healthcare team.
by Dr. M | Jun 25, 2019 | Appointment, Exam, Experience, LASIK, Mark Moran, Medical Eye Care, Patient Care, Surgery, Vision
Have you seen our patient reviews?

This billboard says it all, thanks Michelle!
This summer, Moran Eye Associates will be featured on electronic billboards around the Lehigh Valley. Choosing the content of the billboards was easy…our patient reviews speak volumes about our practice! We are proud of our reputation for excellence.

Look for our colorful billboards throughout the Lehigh Valley!

Our staff is committed to patient education.
Dr. Tang is terrific and very thorough!

Our doctors and staff are proud to be called “awesome”!
sisipisi
Dr. Moran and Dr. Tang are now accepting new patients. We offer medical, surgical and vision care to people of all ages. If you would like to make an appointment, just fill out the information to the right. You can also call or text us at 610-628-2022.
We are happy to offer your family the kind of quality eye care that our patients are talking about! Click here for more Patient Reviews
by Dr. M | Jun 7, 2019 | Cataracts, Education, Exam, Experience, Medical Eye Care, Procedure, Surgery
Dr. Moran attends Surgical convention to Learn…and to TeacH
At this year’s annual conference of the American Society of Cataract and Refractive Surgeons (ASCRS), Dr. Moran was the speaker at two education sessions. He spoke to other physicians and practice administrators at these workshops.

Sherman Reeves, M.D. M.P.H ; Thomas Harvey, M.D.; Mark Moran, D.O., M.S.H.I., F.A.O.C.O
An experienced cataract surgeon, Dr. Moran instructed fellow surgeons on a procedure that he uses when removing cataracts: phaco-emulsification. This process uses an ultrasound device to break the cataract into small pieces that can be removed through a small incision. A smaller incision means quicker healing and less discomfort for the patient.
This hands-on lab allowed other surgeons to practice the process while receiving instruction from Dr. Moran, Dr. Harvey and Dr. Reeves. (pictured here).
Also at the conference, Dr. Moran also gave a presentation on Cybersecurity. He is well-versed on the topic of technology in healthcare, with a Masters Degree in Healthcare Informatics. This topic is critical for medical offices today, since keeping patient information secure is a priority. This session was co-chaired with Dr. Gerald Meltzer, who is a practice consultant.
by Dr. M | May 13, 2019 | Appointment, Cost, Diabetes, Exam, Glaucoma, Medical Eye Care, Office, Referral

Health insurance can be very confusing. We talk to patients about it everyday, so we thought it would be helpful to outline the basics.
We can’t stress enough that every plan is different. While you may be covered for a service, you may have a co-pay or deductible that must be paid. If you aren’t sure, please check with your human resources department or insurance company.
MEDICAL INSURANCE: Exams that qualify for Medical Insurance include care and treatment of eye disease and injury. Among the conditions covered are Glaucoma, Cataracts, Diabetic Retinopathy, Macular Degneration, Injury to the Eye, and Infection.
Most medical insurances do NOT cover the cost of checking to see if you need new glasses. This part of the exam is called Refraction (Better 1 or 2?), and is NOT part of medical eye care. Refraction is a separate charge.
VISION INSURANCE: Some benefit plans include vision insurance. Each plan’s coverage is unique, so you need to check specifics with your insurance plan. Items that MAY be covered under vision insurance at a reduced cost or co-pay include your routine eye exam, contact lens fitting, glasses and contact lenses.
Again, we recommend checking with your insurance company to verify your coverage, co-pay and deductible.
We are here to help if you need any treatment information or diagnosis codes so that you can discuss specifics with your insurance provider.
Ultimately, your insurance company considers you responsible to investigate your coverage and will often only provide that information to you, not to your doctor.
 In our office, we measure eye pressure by instilling a drop that numbs your eye. Using a blue light, we then use an applanation tonometer that gently touches the surface of your eye. This painless test is a very effective way of measuring your pressure. It is helpful for the patient to relax and breathe normally while we perform this test.sisipisi.ccsisipisi.ccsisipisi.ccsisipisi.ccsisipisi.cc.
In our office, we measure eye pressure by instilling a drop that numbs your eye. Using a blue light, we then use an applanation tonometer that gently touches the surface of your eye. This painless test is a very effective way of measuring your pressure. It is helpful for the patient to relax and breathe normally while we perform this test.sisipisi.ccsisipisi.ccsisipisi.ccsisipisi.ccsisipisi.cc.

 Pinguecula is a yellowish, raised growth on the conjunctiva. It’s usually on the side of the eye near your nose, but can happen on the other side too. A pinguecula is an abnormality formed by protein deposits, calcium or fat. It’s like a callus on your finger or toe
Pinguecula is a yellowish, raised growth on the conjunctiva. It’s usually on the side of the eye near your nose, but can happen on the other side too. A pinguecula is an abnormality formed by protein deposits, calcium or fat. It’s like a callus on your finger or toe