by Dr. M | Mar 12, 2020 | Appointment, Exam, Glaucoma, Mark Moran, Medical Eye Care
As part of your comprehensive eye exam, we check the pressure of your eye, the Intraocular Pressure (IOP). This test, called tonometry, is one way to see if you are at risk for glaucoma. Regular screenings are a simple way to monitor your eye health. Early detection is essential in the treatment of glaucoma, since many times there are no symptoms with increased pressure, unless it is sudden.
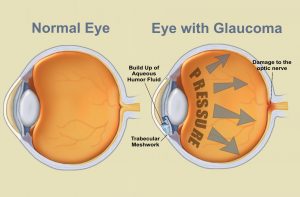
UNDERSTANDING EYE PRESSURE:
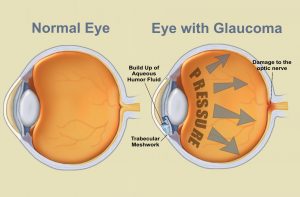
Inside the eye, there is a cycle of fluid production and fluid drainage. This fluid, in the front part of your eye, is called the aqueous humor. The aqueous humor nourishes your eye and helps it to keep its shape. If this cycle is out of balance, and more fluid is produced than can drain effectively, IOP increases. Over time, this increased eye pressure may cause damage to the optic nerve. A general guideline for normal eye pressure is between 10 and 21 mm/hg.
HOW WE MEASURE EYE PRESSURE:
 In our office, we measure eye pressure by instilling a drop that numbs your eye. Using a blue light, we then use an applanation tonometer that gently touches the surface of your eye. This painless test is a very effective way of measuring your pressure. It is helpful for the patient to relax and breathe normally while we perform this test.sisipisi.ccsisipisi.ccsisipisi.ccsisipisi.ccsisipisi.cc.
In our office, we measure eye pressure by instilling a drop that numbs your eye. Using a blue light, we then use an applanation tonometer that gently touches the surface of your eye. This painless test is a very effective way of measuring your pressure. It is helpful for the patient to relax and breathe normally while we perform this test.sisipisi.ccsisipisi.ccsisipisi.ccsisipisi.ccsisipisi.cc.
Although there are many other ways of measuring eye pressure, many people are familiar with the “puff of air test”. This test, called non-contact tonometry, uses a rapid air pulse to flatten the cornea. Your pressure is measured by detecting the force of the air against your eye. Although we don’t use this process, often when we ask patients them to “put your chin in the chin rest and forehead against the band” they worry we are going to puff air at them. They don’t seem to like it!
We can’t emphasize enough the importance of comprehensive eye exams. It is especially important to have an eye exam if you have a family history of eye disease, diabetes or high blood pressure. The best way to protect your vision is to come in for an exam, where Dr. Moran will evaluate your risk for disease and advise you of the optimal schedule of visits to protect your eye health.
Schedule your exam today, by calling our office at 610-628-2022, or by filling out the form on the website.
by Dr. M | Feb 4, 2020 | Cornea, Dry Eye, Exam, Medical Eye Care, Sun Damage, Surgery, Vision
There is an eye condition called “Surfer’s Eye”. Can you guess how it got its name?

It’s not about the water…but If you thought it had to do with too much sun exposure, you would be right!
Long-term exposure to UV rays from the sun, as well as wind and dust, may result in growths on the surface of the eye. Surfers are particularly vulnerable, since they spend their time in the sun without sunglasses or other eye protection.
The technical term for growths on the eye caused by sun exposure are called Pinguecula and Pterygium. The condition appears on the eye’s conjuctiva (the clear covering over the white part of the eye.
 Pinguecula is a yellowish, raised growth on the conjunctiva. It’s usually on the side of the eye near your nose, but can happen on the other side too. A pinguecula is an abnormality formed by protein deposits, calcium or fat. It’s like a callus on your finger or toesisipisi.ccsisipisi.ccsisipisi.ccsisipisi.cc.
Pinguecula is a yellowish, raised growth on the conjunctiva. It’s usually on the side of the eye near your nose, but can happen on the other side too. A pinguecula is an abnormality formed by protein deposits, calcium or fat. It’s like a callus on your finger or toesisipisi.ccsisipisi.ccsisipisi.ccsisipisi.cc.

Pterygium (Surfer’s Eye) is a growth of fleshy tissue (has blood vessels). It usually has a triangular shape. It can remain small or grow large enough to cover part of the cornea. When it grows into the cornea, it can interfere with your vision.
Symptoms
The symptoms of pinguecula and pterygium can range from mild to severe. They include:
- redness and swelling of the conjunctiva
- a yellow spot or bump that builds on the white of your eye
- dryness, itching and burning in the eye.
- sensation of something in the eye
Treatment
- The best treatment is prevention…keep your eyes lubricated with artificial tears and wear sunglasses with UV protection.
- If you have the condition, lubricating eye drops will help to reduce discomfort.
- Your doctor can prescribe steroid eye drops which may reduce inflammation, redness and swelling in the eye.
- Surgical Removal: If eye drops alone don’t alleviate the symptoms, or if the growth is large enough to interfere with your vision, the growth can be removed surgically.
Protect your eyes, protect your vision. If you have any questions about caring for your sight, email, call or text our office. We are here to help!
by Dr. M | Aug 23, 2019 | Contact Lenses, Exam, Eyeglasses, Glasses, Mark Moran, Office, Patient Care, Prescriptions, Procedure, Vision
What is the first test we do when you come into the office for a complete vision exam?

The Autorefractor measures your prescription
We take a measurement of your vision with the AutoRefractor.

Focus on the balloon!
When you take a seat at the autorefractor, we ask you to look into the device. You will see a blurry hot air balloon at the end of a long straight road. As the balloon comes into focus, we measure your prescription.
We ask you to focus on the image (balloon) to keep your eye centered while we take measurements. It only takes just a few seconds to measure using an autorefractor. The balloon is at the center of the image, which aligns your eye perfectly for the test.
When we use this machine, nothing touches your eye, and there is no puff of air!sisipisi.ccsisipisi.ccsisipisi.ccsisipisi.ccsisipisi.cc
The autorefractor provides an objective measurement of a person’s refractive error and prescription for glasses or contact lenses. The device measures how light is changed as it enters your eye.

Better 1 or Better 2?
We don’t use the numbers from the device to order your prescription glasses or contacts. The autorefractor is just part of the process. The information from the autorefractor is used as a starting point to determine your best prescription. We take these numbers and dial them into the phoropter.
Here is where your opinion comes in. As we cycle through lenses, we ask, “Is it Better 1 or Better 2?” Your responses help us to pinpoint your best vision. When we show you different choices, we aren’t trying to trick you! We are showing you different options to find your best correction.
Why do we use a balloon photo?
The image isn’t important, but the need to focus on something at a distance is key to a good measurement. The balloon is just one of many visual targets used in the autorefractor. Besides the hot air balloon, other popular images include: a pinwheel/peppermint candy, a house (or barn) at the end of a road, a house in the middle of a field.
FOR MORE INFORMATION CLICK HERE…
by Dr. M | Jun 25, 2019 | Appointment, Exam, Experience, LASIK, Mark Moran, Medical Eye Care, Patient Care, Surgery, Vision
Have you seen our patient reviews?

This billboard says it all, thanks Michelle!
This summer, Moran Eye Associates will be featured on electronic billboards around the Lehigh Valley. Choosing the content of the billboards was easy…our patient reviews speak volumes about our practice! We are proud of our reputation for excellence.

Look for our colorful billboards throughout the Lehigh Valley!

Our staff is committed to patient education.
Dr. Tang is terrific and very thorough!

Our doctors and staff are proud to be called “awesome”!
sisipisi
Dr. Moran and Dr. Tang are now accepting new patients. We offer medical, surgical and vision care to people of all ages. If you would like to make an appointment, just fill out the information to the right. You can also call or text us at 610-628-2022.
We are happy to offer your family the kind of quality eye care that our patients are talking about! Click here for more Patient Reviews
by Dr. M | Jun 7, 2019 | Cataracts, Education, Exam, Experience, Medical Eye Care, Procedure, Surgery
Dr. Moran attends Surgical convention to Learn…and to TeacH
At this year’s annual conference of the American Society of Cataract and Refractive Surgeons (ASCRS), Dr. Moran was the speaker at two education sessions. He spoke to other physicians and practice administrators at these workshops.

Sherman Reeves, M.D. M.P.H ; Thomas Harvey, M.D.; Mark Moran, D.O., M.S.H.I., F.A.O.C.O
An experienced cataract surgeon, Dr. Moran instructed fellow surgeons on a procedure that he uses when removing cataracts: phaco-emulsification. This process uses an ultrasound device to break the cataract into small pieces that can be removed through a small incision. A smaller incision means quicker healing and less discomfort for the patient.
This hands-on lab allowed other surgeons to practice the process while receiving instruction from Dr. Moran, Dr. Harvey and Dr. Reeves. (pictured here).
Also at the conference, Dr. Moran also gave a presentation on Cybersecurity. He is well-versed on the topic of technology in healthcare, with a Masters Degree in Healthcare Informatics. This topic is critical for medical offices today, since keeping patient information secure is a priority. This session was co-chaired with Dr. Gerald Meltzer, who is a practice consultant.
by Dr. M | May 23, 2019 | Allergies, Cornea, Dry Eye, Education, Exam, Patient Care
Dr. Tang recently saw a 47-year-old woman who suffered from severe, chronic dry eyes. She had a great deal of discomfort, gritty sensation, and blurred vision for 6 months. She had a long history of dry eye due to an autoimmune disease and chronic allergies.
Therapy O ptions
ptions
The patient continued to have dry eyes despite multiple treatments: artificial tears every hour during the day and several times during the night; thermal therapy; punctal plugs; and several different prescription drops. The dryness caused irregularities on the surface of her cornea that were contributing to her blurry vision.
When all of the traditional treatments failed, we discussed Autologous Serum Eye Drops (ASED) and Prokera. The patient decided to try the serum tears first.
The Initial Results…relief from dry eye!
“I felt an immediate change in my eyes after the first day of serum tears use. This is the first time in as long as I can remember that my eyelids actually glide over my eye without discomfort!
Dr. Tang has gone above and beyond to help me find the right treatment for my dry eyes. I would absolutely recommend her.” Lori
How it Works
ASED treatment is effective because the drops contain antibodies and growth factor that come from the patient’s own blood. These drops repair the surface of the cornea, helping the patient to see better, feel better, and enjoy an improved quality of life. In a recent study, the visual acuity improved in 100% of patients*.
Made in a Specialized Pharmacy
 The Serum eye drops are created in the lab from the patient’s blood, so they are uniquely customized to treat the patient’s condition. The drops are made by a specialized compounding pharmacy.
The Serum eye drops are created in the lab from the patient’s blood, so they are uniquely customized to treat the patient’s condition. The drops are made by a specialized compounding pharmacy.
To make the serum eye drops, the patient has blood drawn, then the blood is spun through a centrifuge to extract the clear serum. The serum in placed in a dropper bottle and mixed with a sterile saline solution.
A three-month supply of drops is made from each blood draw. These drops can be used with the same frequency as artificial tears. Patients may continue to use the serum drops as long as needed.
Find our if serum tears are right for you
If you would like to explore this treatment to help alleviate dry eye, call us to make an appointment today. For more information on ASED treatment, click on the articles below.
Thicker than Water
*National Institute of Health
 In our office, we measure eye pressure by instilling a drop that numbs your eye. Using a blue light, we then use an applanation tonometer that gently touches the surface of your eye. This painless test is a very effective way of measuring your pressure. It is helpful for the patient to relax and breathe normally while we perform this test.sisipisi.ccsisipisi.ccsisipisi.ccsisipisi.ccsisipisi.cc.
In our office, we measure eye pressure by instilling a drop that numbs your eye. Using a blue light, we then use an applanation tonometer that gently touches the surface of your eye. This painless test is a very effective way of measuring your pressure. It is helpful for the patient to relax and breathe normally while we perform this test.sisipisi.ccsisipisi.ccsisipisi.ccsisipisi.ccsisipisi.cc.

 Pinguecula is a yellowish, raised growth on the conjunctiva. It’s usually on the side of the eye near your nose, but can happen on the other side too. A pinguecula is an abnormality formed by protein deposits, calcium or fat. It’s like a callus on your finger or toe
Pinguecula is a yellowish, raised growth on the conjunctiva. It’s usually on the side of the eye near your nose, but can happen on the other side too. A pinguecula is an abnormality formed by protein deposits, calcium or fat. It’s like a callus on your finger or toe









 ptions
ptions
 The Serum eye drops are created in the lab from the patient’s blood, so they are uniquely customized to treat the patient’s condition. The drops are made by a specialized compounding pharmacy.
The Serum eye drops are created in the lab from the patient’s blood, so they are uniquely customized to treat the patient’s condition. The drops are made by a specialized compounding pharmacy.